I was recently recruited by a friend of mine to join him in a 31-day pushup and body squat challenge through which we would be working our way up to completing 750 body squats and 200 pushups in a single day. I have to admit that I was skeptical as to whether this would be possible.
The challenge was broken into 3-day segments, where we would perform increasing reps over the course of the 3 days, with the 4th day being our rest day.
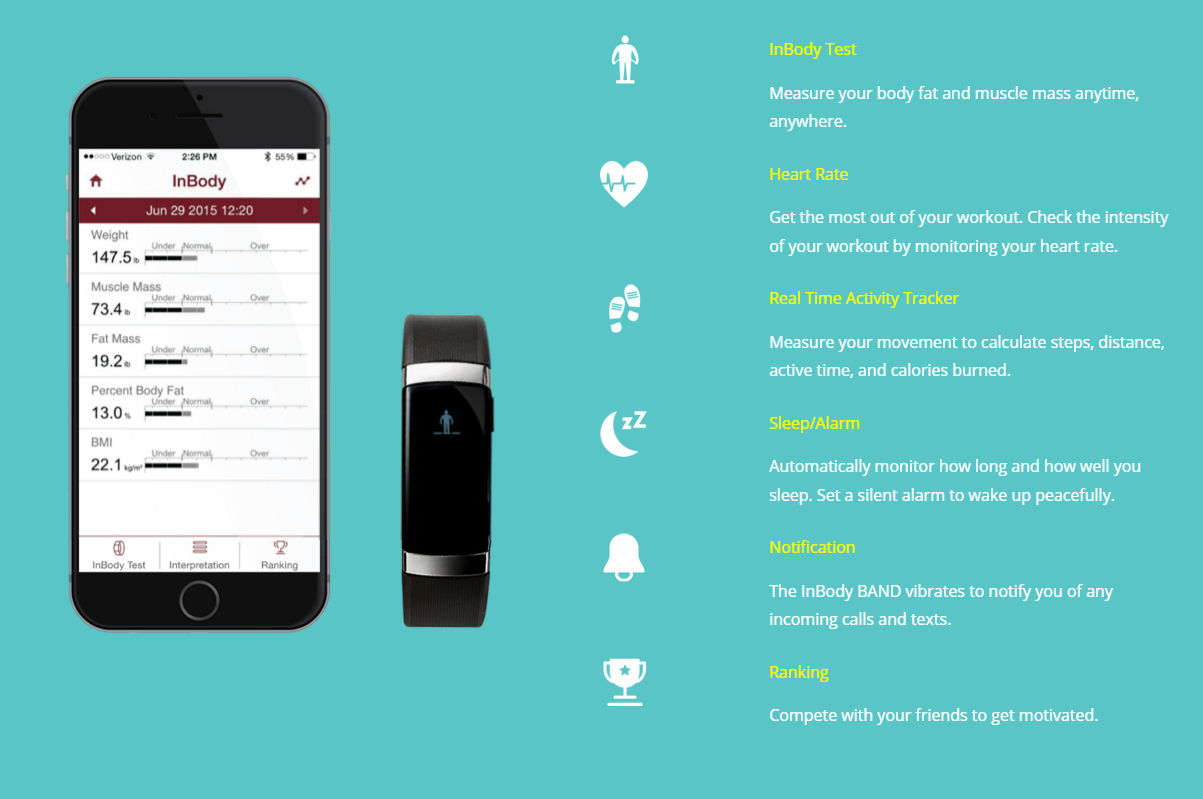
I’d recently begun wearing the new InBody Band which unlike most health trackers, also captures full body composition readings, such as body fat %. Being equipped with a new tracker I thought it would be an interesting test to see how this new regiment would actually affect my body composition.
The Good
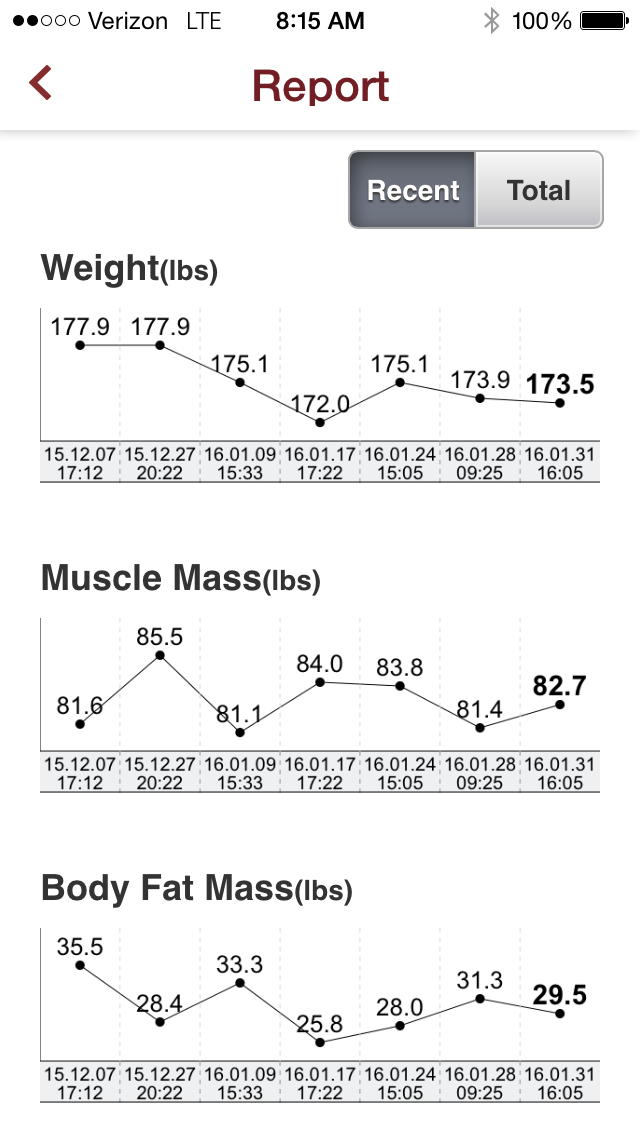
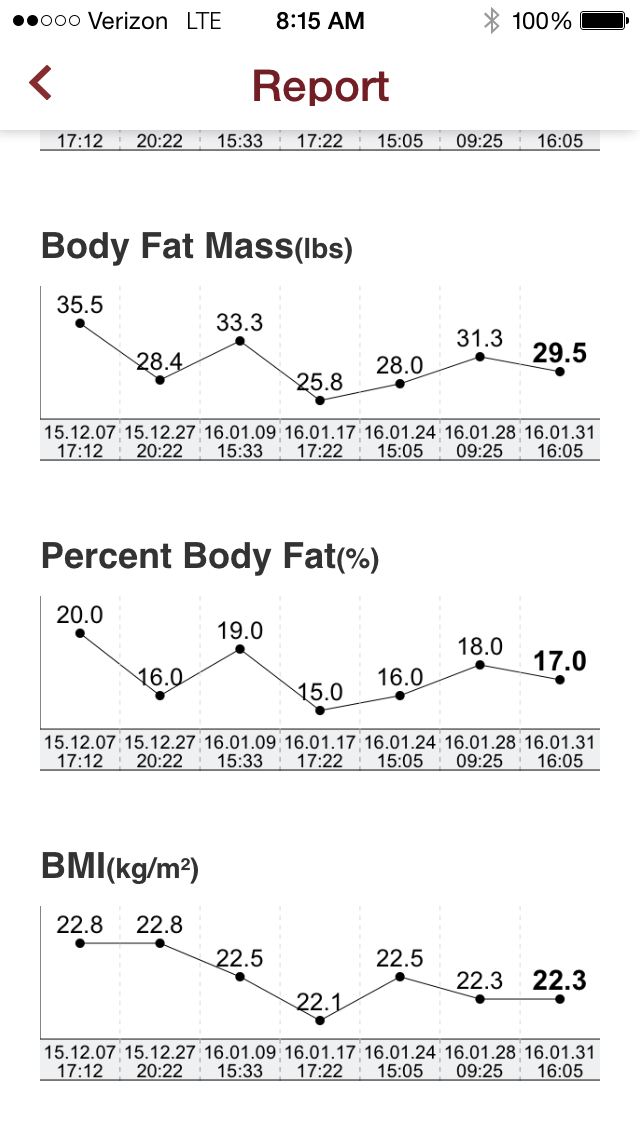
I can confirm that I did indeed see changes in my body composition: body fat %, muscle mass, fat mass, etc, but I also felt like the “challenge” itself was a fresh new approach for me to try and get back into shape.
I was encouraged by the results I was able to see each week when I’d perform a new body composition test. In my opinion this is the most compelling device I’ve seen, as it actually performs a function unmatched by my smartphone, AND it helps me understand how this activity is actually affecting my body.
I was able to drop my body fat by +- 6lbs (+-3% lost)
I'm the type a person who loves being able to monitor progress, so I looked forward to the weekly body composition test to see what was really happening in there, as BMI and weight don't mean much to me. I was a D1 athlete in a previous life, so this platform provided a nice motivational boost to make the challenge a little more fun.
Here’s the thing, though. Mobile health has come under scrutiny as recent reports have highlighted mixed results in which mobile health was used with participants, begging the question of while health tracking CAN be a great resource for those who already possess motivation for change, can it ALSO be used to benefit those who really need it (i.e. those suffering from chronic disease)?
The Bad
Yes, these tools allow us to gain better understanding of how we are progressing but they provide very little in terms of ongoing accountability (hence, why many devices go unopened or find their way into drawers and forgotten).
For example, in January, the Scripps Translational Science Institute published their “Wired for Health” Study which was intended to uncover whether equipping patients suffering from certain chronic conditions with mobile health tools would result in any type of significant outcomes or cost savings.
160 patients with conditions, such as hypertension or diabetes, were split into an intervention and control group, where members of the intervention group were issued an iPhone 4 and mobile health device respective of their condition: Withings blood pressure monitor for those with hypertension, etc.
Many were shocked to learn that the study showed NO difference between the two groups.
Scipps announcement shared by mobihealthnews.com
With that said, it’s worth digging deeper to explore the possible factors behind these results:
1. The study only reviewed data over 6 months which may have been too brief a duration to see real results.
2. Being that the study took place in 2013-2014, advancements in health tracking technology through the likes of passive data collection and more user friend interfaces could potentially have enhanced patient experience.
3. While coaches and nurses were made available to the patients, usage was not mandatory. [Keep this point in mind...]
The Hard Truth
Mobile health has a dirty little secret that is starting to be recognized across the market. Health tracking platforms alone have a difficult time influencing the lifestyle habits of users.
Why?
First off, it requires a user with a sense of motivation to overcome some of the key hurdles associated with health tracking to begin with: keeping a device charged, remembering to put it back on after charging, etc. That process becomes annoying over time, and can be a significant deterrent for those half-heartedly trying to meet a fitness goal. I can admit that I even struggle to keep my device charged all the time.
Secondly, in some instances traditional consumers are left not fully understanding how to read the data being captured, understand when it’s meaningful, or even apply the information to their daily lifestyle. For instance, the latest generation of wearables have included heart rate tracking which I’ve heard firsthand from health and wellness professionals both, who’ve expressed concerns with client or patient understand.
For the most part, mobile health has seen the majority of its success up to this point through enabling the intrinsically motivated to monitor their progress and provide reminders when there is present risk of him or her veering off course.
What about the rest of society or those trying to manage chronic conditions?
There's Hope
The Scripps study was correct in highlighting that mobile health alone is not the solution, but they underestimated one of the key factors in the study’s failure.
Not requiring patients to interact will a health professional (i.e. coach or nurse) throughout the duration of the study was the study’s primary pitfall.
Look at it this way. How effective do you think schools would be if students were simply handed text books and were expected to work through the curriculum alone? Some students would thrive, but the majority would find themselves frustrated and in need of additional context or help from a professional – i.e. the teacher.
The likelihood for success of any lifestyle program is dramatically enhanced when the technology is paired with a professional to help provide understanding and additional accountability.
Data is only significant to the user if they can clearly see WHY it is meaningful, WHERE their numbers SHOULD be, and WHAT they can do to improve.
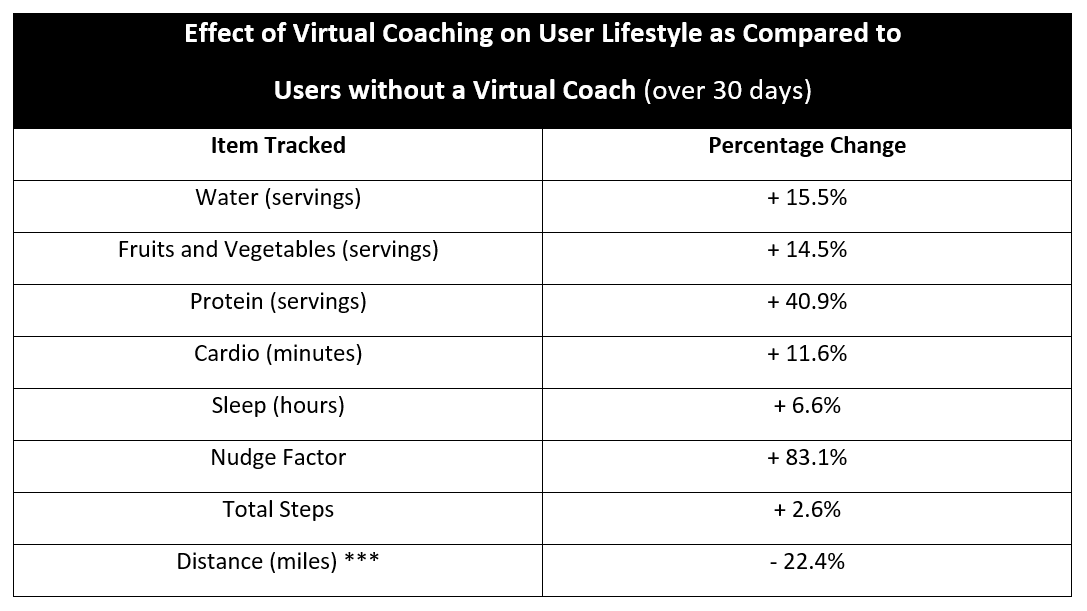
Over the past few months we’ve had a chance to dive into the data collected on our platform, Nudge, more specifically reviewing the differences in user behavior between non-coached users vs. users working with a healthcare professional.
www.nudgecoach.com
Nudge and Nudge Coach allow for virtual care management through the use of health tracking apps, custom tracking, and touchpoint management, helping practitioners better manage more patients or clients. Users can sign up on the Nudge app regardless of whether they are or are not working with a professional.
Several quick notes on the comparison…
- Those tracking nutrition or hydration are tracking based on servings.
- The Nudge Factor is our proprietary lifestyle score analyzes total lifestyle data over a 30-day period. This score allows for objective comparison and helps identify client/patients maybe needing additional attention.
- Distance tracked is expected to be lower, as those working with a professional are less likely to be fitness enthusiasts.
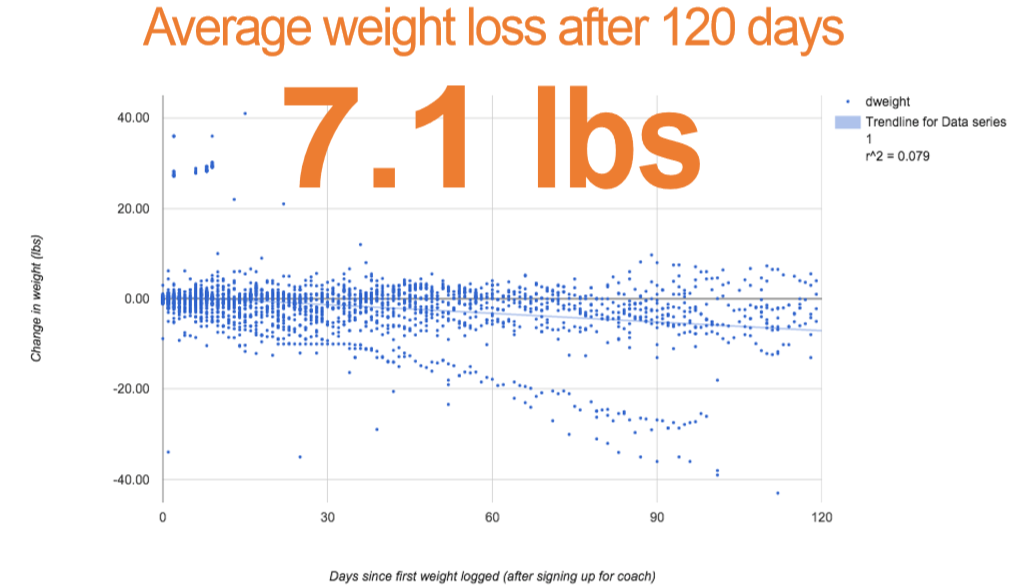
Currently, weight is one of the best indicators of outcomes on the system and you will also see that those working with a professional on average have lost over 7 lbs through 120 days.
However, It’s worth noting that certainly not every user working with a professional NEEDS to lose weight, so while there are certainly instances of people losing upwards of 100 lbs on the system, or none at all, this is simply highlighting the overall trend of this managed population.
Coached individuals have lost over 7 lbs. on average over 120 days.
While success can be achieved through personal use of mobile health devices, all of our data suggests the importance of including the human component: the health or wellness professional.
This person helps users overcome some of the basic hurdles to ensure user compliance and engagement over time, addressing frustrations and recognizing underlying issues that may need additional attention.
Where health tracking has gained a majority of its attention through the consumer market, we are entering an era where these devices are becoming vehicles to better care and a more streamlined care system.
There is still plenty of work ahead, but ultimately the best way to enhance long term engagement and outcomes using mobile health is first and foremost to make sure we don’t try and eliminate the human component of care management.
Without adoption from health and wellness professionals it looks like mobile health will continue to be a nice-to-have solution for motivated consumers, and miss out on the larger picture of helping fill the void in patient and client care.